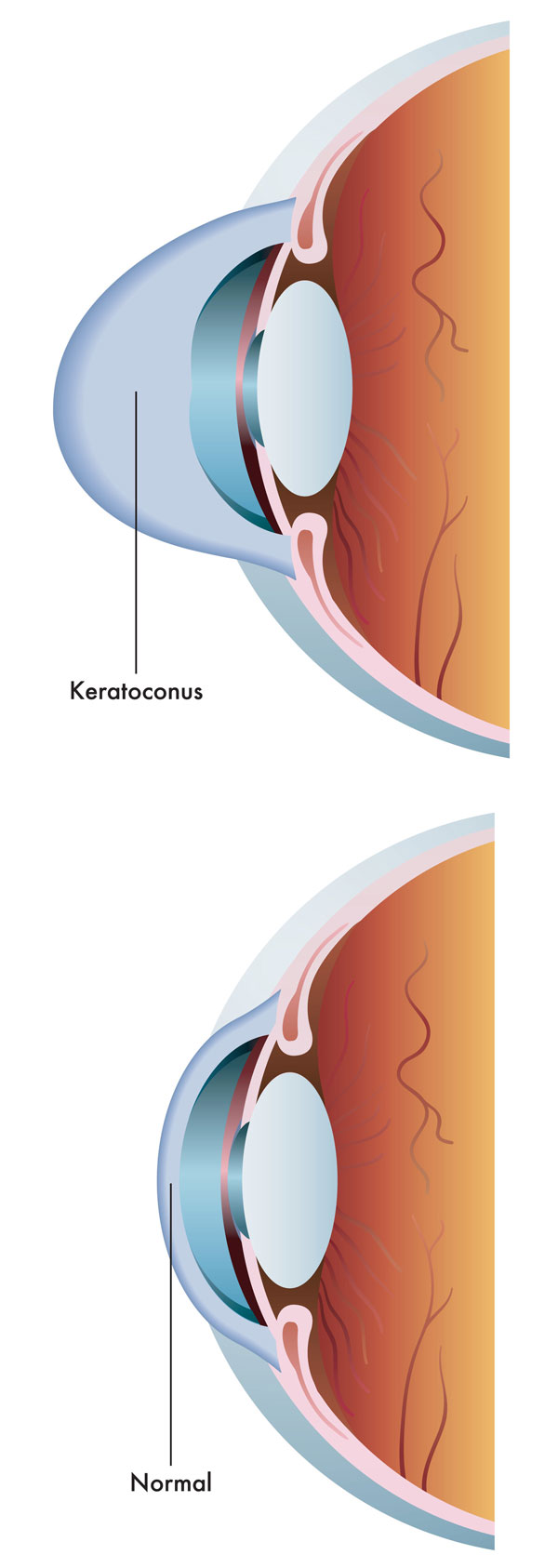
Keratoconus: is a disease that makes the cornea weak causing it to bulge outward. Most often, this bulging is in the lower half of the cornea and first presents progressive diminution of vision due to myopia (near sightedness) and astigmatism. In mild or early stages of Keratoconus, eyeglasses may correct the vision.
The possible treatment options for Keratoconus
There is no cure for Keratoconus and the only treatment is at improvement of the refractive errors induced by the disease.
In more advanced cases the Keratoconus rigid contact lenses may be required to improve visual acuity; however they can not stop disease progression.
Until on recant, the only therapeutic option for advanced cases with significant reduction of visual acuity was corneal transplantation (penetrating keratoplasty).
In the past few years, a new procedure has been developed that is supposed to stop the progression of Keratoconus This procedure is called Corneal collagen cross linking.
CORNEAL collagen CROSS LINKING "CCL" FOR TREATMENT OF KERATOCINUS
The aim of this procedure is to stabilize the corneal and prevent the progression of Keratoconus.
It is a non-invasive procedure that has been proven to strengthen the weak corneal structure in Keratoconus. This method works by inducing cross linking of the corneal collagen bundles, which are the natural "anchors" within the cornea.
These anchors are responsible for preventing the cornea from further bulging and becoming irregular (which is a cause of Keratoconus).
The corneal cross linking treatment is performed in our center and is a one-time treatment.
During the treatment, riboflavin eye drops are applied to the cornea, which is then activated by a special light. This is the process that has been shown in laboratory and clinical studies to increase the amount of collagen cross-linking in the cornea and strengthen the cornea. In published European studies, such treatments were proven safe and effective in patients.
After the treatment a bandage contact lens is applied and a combination of a steroid and antibiotic drop is prescribed.
In Approximately 80% of the patients regression of the Keratoconus could be seen. No unwanted side effects such as specification of the lens or loss of endothelial cells has been reported.
Only during the first 2 to 3 months after the cross linking a slight superficial corneal haze has been noticed.
Generally this minor haze disappears with any treatment, but a supportive therapy with soothing this minor or with a local steroid can be used.
In conclusion. Early treatment with this procedure will enormously reduce the need for future corneal transplantation for many of the Keratoconus patient. It will be a great relief to our current shortage of available corneal tissue for transplantation.